Reconstruction Non-reconstruction Experiences
Breast reconstruction is the option many women choose after mastectomy but it isn't the only option.
 Breast reconstruction is the option many women choose after mastectomy, but it isn't the only solution.
Breast reconstruction is the option many women choose after mastectomy, but it isn't the only solution.
Many factors influence the decision of whether or not to have reconstructive surgery, and each woman must evaluate those factors for herself. Sometimes it helps to hear from other women about why they made the choices they made, and how they feel down the road. Some of our friends have shared their breast surgery stories.
Mastectomy on One Side with Reconstruction
Making a breast reconstruction decision can be complicated for a woman who has only one breast removed. Both of the friends I spoke with for this part of the article have had problems with their reconstruction. Not all women have problems with their reconstruction, but their stories do highlight some of the potential difficulties.
Rebecca G. from New York
Rebecca had reconstruction at the time of her mastectomy. She did her homework prior to making the decision:
 “I spoke to two plastic surgeons. I attended a
“I spoke to two plastic surgeons. I attended a
reconstruction group at SHARE (a resource center in New York for breast and ovarian cancer) and another support sponsored by JALBCA (Judges and Lawyers Breast Cancer Action).”
However, the procedure was more uncomfortable than she had expected. “The tissue expander felt like a weight in my chest. It was really uncomfortable physically and emotionally. There was a point when I wondered if doing the reconstruction at the same time as the mastectomy was really such a good idea.”
Rebecca has had to adjust to the results:
“I am not great with scars. I could not look at the reconstructed breast for a long time. Everyone tells me it’s a great job. I think it is okay.
“One difficulty that often comes up is that the natural breast does not match the reconstructed breast. “If you gain weight,” Rebecca explains, “the saline implant can be a problem. When I gain weight, my natural breast gets bigger and the reconstructed breast does not. Everyone thought that would help me maintain my weight. They were all wrong.
“I never had the nipple done. I’ve had enough ‘stuff’ done to my breasts. It’s my husband’s sense of humor that has really helped me. He calls my reconstructed breast ‘the bionic boob.'”
 Rebecca explains her decision to have a lift on the other side a couple of years later:
Rebecca explains her decision to have a lift on the other side a couple of years later:
“Apparently they can put a person on the moon but they can’t create a sagging 47-year-old breast — only perky 17-year-old breasts. My plastic surgeon suggested that I have the other breast lifted to match. My breasts had always been pendulous. I rememb
er the plastic surgeon saying that I could have great cleavage after the reconstruction. I had always wanted cleavage but my breasts were too far apart.
“I asked all of my doctors (oncologist, radiologist, surgeon, and gynecologist) whether the lift would in any way affect follow-up on the “healthy” breast. All of them agreed that it would be fine.”
But the results of the lift were disappointing. “It was much more painful than I expected. There was a chance that I would lose feeling in that breast as well. I don’t know why I let the plastic surgeon talk me into this. I let him cut into a perfectly healthy breast. It didn’t look like my breast anymore. I guess I thought that after the lift I’d be 'normal', whatever that means. Instead, I felt like I had lost both breasts.
“My husband is the only one I’m usually naked around and he doesn’t care. So what if I had one perky breast and one sagging breast? I think it bothered the plastic surgeon more than it would have ever bothered me.
“A few months after the surgery, the radiologist told me my 'crystal clear right breast' had many areas that he wanted to biopsy, based on his inability to tell the difference between cancer and scar tissue. The lift was a year ago and I am terrified about the mammogram.”
However, Rebecca has found one benefit: “On the plus side, it’s nice to run out to the store and not have to wear a bra.”
Nancy S. from California
After a biopsy revealed a 2.1 cm tumor in the lower left quadrant of her left breast, Nancy elected to have a mastectomy.
“I actually never considered not having reconstruction. I spoke with at least eight breast cancer survivors and two plastic surgeons. The first plastic surgeon spent a long period of time discussing options. He did not advocate for any one procedure. He explained the rate of infection with implant placement at the time of mastectomy was higher than when surgery was deferred to a later date. He was easy to speak with, and took my mind off cancer and onto cosmetic considerations. The second plastic surgeon was a big proponent of abdominal flap surgery. He showed me numerous pictures of the procedure which were very upsetting to me, as I am a person who doesn’t do well looking at blood and incisions, etc.
“All this focus on reconstruction was possible because the likelihood of nodal involvement was slim. My tumor markers were not indicative of more advanced disease. Chemotherapy was lightly mentioned as an option because of my age (49). I was told that the choice of a mastectomy also eliminated the need for radiation (a treatment which certainly would have changed my choice to have implants put in at the time of the initial surgery).
 “I chose to have an implant put in at the time of the mastectomy. When bandages were removed the day after surgery, I was very pleasantly surprised to have some “breast” (my doctor had expanded it with approximately 200 CC of saline). It certainly made the shock of a mastectomy easier. I was very pleased with my choice.”
“I chose to have an implant put in at the time of the mastectomy. When bandages were removed the day after surgery, I was very pleasantly surprised to have some “breast” (my doctor had expanded it with approximately 200 CC of saline). It certainly made the shock of a mastectomy easier. I was very pleased with my choice.”
Nancy’s pathology report showed nodal involvement, but her chemotherapy was postponed until the drain could be removed. Her breast area continued to drain.
Nancy describes some complications that followed: “I couldn’t start chemo with the drain in place because of infection risk. I asked about having the implant removed so I could get on with chemo and was assured by my oncologist that I could wait up to twelve weeks to start chemo. My plastic surgeon continued bi-weekly expansions in spite of the drain. He would tell me how pleased he was with the appearance of the implant but I didn’t share his enthusiasm. I just wanted it out.
“Finally, after seven weeks, the drainage decreased and the doctor removed the drain. Eight hours later I had 104 fever. After 24 hours of IV antibiotics, the implant was removed. I was glad to get rid of it so I could proceed with chemo and radiation.
“After removing the wrap from surgery a few days later, I realized I had a new concern — I needed a prosthesis. I had not prepared for this situation so I went to the yellow pages and made a stop on the way to work to buy a breast form.
“Do I regret the decision I made? Yes. In hindsight, I should have waited until I knew what treatment was ahead of me. I also should have been more assertive and insisted on removal of the implant. I kept thinking it would eventually improve, but I felt resentful of the plastic surgeon’s emphasis on the appearance of the reconstruction vs. my need to be rid of drains and proceed with treatment.”
“You would think this would have forever eliminated my desire for reconstruction. However, after treatments were complete and time had passed, I realized the prosthesis had always seemed like a “third” wheel. It was always sticky and hot when I played tennis. I couldn’t wear a T-shirt without a bra while working in the garden for fear that a neighbor might stop by to chat.
“Once, while body surfing with my 12-year-old nephew at the beach, I caught a great wave, rode it in, and my prosthesis popped out of my bathing suit. On another occasion when I was shopping for an evening dress for a Christmas party, I realized I couldn’t find a dress in which I could safely 'lean over the punch bowl' unless the neckline was at my collarbone. Eventually these feelings led me to explore reconstruction options a second time. I wanted my ‘freedom’, so to speak.”
Nancy went back to researching her options: “I went to three plastic surgeons with the same question: ‘What is the success rate with an implant placed under radiated skin? What are the complications and what are the percentages of each? How would the end result appear compared to an implant in a non-radiated area?’ (I was unwilling to consider using my own tissue for a flap reconstruction.) The risk of encapsulation was 20% and the end result would not be as soft with radiated skin, possibly making it more difficult to match. I did a lot of reading and felt comfortable with a success rate of approximately 80%. I decided to have the implant and match the reconstructed breast with a lift on the other side.
“Expansion over a six-month period went smoothly. Placement of the saline implant and breast lift were without incident until I experienced capsular contraction about six weeks after surgery. It has been downhill since then. The encapsulated implant had to be removed a year later. Complications have also arisen since that surgery leading to another surgery, a capsulectomy, in the near future.”
Nancy maintains a good attitude. “I know that I made informed choices and accept that I was one of the 20% who had complications. I just credit them to bad luck. I miss having the option for reconstruction and I miss the brief freedom I experienced when the implant allowed me more options for dressing and not wearing bras. However, I know now that I will not have further reconstruction and that living with a prosthesis is just fine from here on out.”
Mastectomy on One Side with No Reconstruction
Rose O. from California
Rose had a mastectomy in Sept of 1994. She describes her situation: “The question of reconstruction didn’t come up in any of my doctor visits. I didn’t know I could have reconstruction at the same time as the mastectomy, so I assumed that the question of reconstruction would come later.”
 She ended up not going back for reconstruction surgery. Rose says her biggest problem is balance. She describes her recent thoughts about that: “I have never wished I’d chosen reconstruction, but I don’t like how unbalanced my body is. My remaining breast is large, so it can be a problem at times.
She ended up not going back for reconstruction surgery. Rose says her biggest problem is balance. She describes her recent thoughts about that: “I have never wished I’d chosen reconstruction, but I don’t like how unbalanced my body is. My remaining breast is large, so it can be a problem at times.
“My plastic surgeon mentioned recently that I might consider reconstruction to give my body more balance. I told him I was not interested in having more surgery. He responded that he wasn’t trying to talk me into it, he just wanted me to think about it. I got some literature on reconstruction, but after reading it I’ve decided I would rather have the other breast removed. I don’t know if my insurance would cover it since it’s not a reconstruction. I haven’t looked into that yet. I think that if I could be sure an implant would be safe and not encapsulate or something like that, I might consider reconstruction. Right now I’m not ready to take the risk.”
Sometimes, Rose points out, living with a prosthetic can be pretty amusing:
“Something funny happened just a couple of weeks ago. I was at home at the computer and I wasn’t wearing a bra with a pocket, so my prosthetic kept slipping into the middle of my bra. It was driving me crazy, so I removed it and threw on the dresser.
“I was babysitting my three-year-old grandson at the time and I forgot he was in the room with me. Well, his eyes got really big and he walked to the dresser and poked it with his finger. He ran to my husband and said,’Grandpa, I touched it! Ewww!’”
In spite of her momentary embarrassment, Rose feels comfortable being a one-breasted woman: “I think that my husband’s total acceptance of me whether I have one breast or two has been very important in my comfort with the changes in my body. After seven years of having one breast, it just became who I am. I like to say I have battle scars, but I won the war against breast cancer.”
Bilateral Mastectomies with No Reconstruction
Lynne D. from Canada
Lynne had a lumpectomy initially and then, when the pathology report came back showing that she needed further surgery, she chose to have bilateral mastectomies. She chose not to have reconstruction.
“Basically, I would have breasts — which in our society are viewed as more sexually attractive. I could wear lower cut clothing, regular bathing suits, and regular bras, without the fear of my bra riding up.
“But I did not want any more unnecessary surgery. Saline implants involve not only the initial surgery, but very likely more surgery down the road if there is hardening, scar tissue, or leakage. The reconstructed breasts would not look the same as my natural breasts. Flap reconstruction involves much more surgery and I was not willing to consider the pain, the risks of infection, nor the scarring. (Although I did think the tram flap tummy tuck might be a nice option.) I felt reconstruction of any type would make detection much more difficult.”
Bilateral Mastectomies with Reconstruction
Pamela S. from California
Pamela had prophylactic bilateral subcutaneous mastectomies over a decade ago. A subcutaneous mastectomy is a skin-sparing surgery where the nipple is left intact and as much of the skin as possible is preserved. “As a woman in my thirties with no evidence of disease, but a strong family history and uninterpretable mammograms, I wouldn’t have had a “traditional” mastectomy, nor would my surgeon have performed one. The only option to me (other than doing nothing) was subcutaneous mastectomy, with the simultaneous placement of a prosthetic under the major pectoralis muscle.
“I got multiple second opinions and researched my options in depth. My plastic surgeon shared his expertise and showed me the results of other patients who had had the procedure. My husband, who is an orthopedic surgeon, was very helpful in the clinical aspects of decision-making and supportive in the emotional aspects.”
More than ten years later, Pamela says: “My concern at the time of my surgery was the cosmetic result. It turns out, I had a very good result. Unless I share my experience, no one would ever know I’ve had mastectomies with reconstruction.”
Barbara D. from California
Barbara had bilateral mastectomies in October 1997, after a second diagnosis of breast cancer. “My grandmother and mother both had breast cancer. My sister chose to have prophylactic mastectomies with reconstruction. I’d seen her reconstruction, so when my cancer came back, I knew I wanted to have mastectomies with reconstruction.”
However, Barbara did not have her reconstruction at the time of her breast cancer surgery. She says:
“I went to see a plastic surgeon before I had the mastectomies and he told me I would have to wait until later to have reconstructive surgery. He confirmed that when I saw him right after my surgery. Apparently, the surgeon had scraped so much of the cancerous breast that it needed time to heal.”
As for Barbara’s results: “Because of all the removal my surgeon did, there wasn’t as much to expand. My plastic surgeon doesn’t believe in filling the sacks full, so the implants can move a bit and look more natural. He created nipples out of skin from my groin. They look very natural. And I definitely have feeling in my skin where the implants are. Apparently not everyone does. I am very happy with my reconstruction. I love not having to wear a bra. I only have one, which I don’t wear too often.”
Making The Decision
As you can see, there are lots of practical and emotional reasons for choosing or not choosing reconstruction. It’s a deeply personal decision. The only “right” choice is one that feels right to you in your particular circumstances. Sometimes circumstances change and you have to re-evaluate your choices, but acknowledging your own feelings is the most important step.
We're here to help
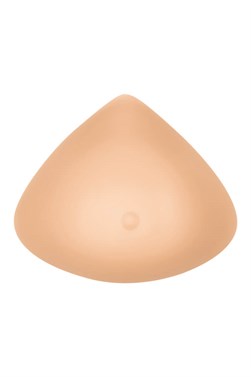
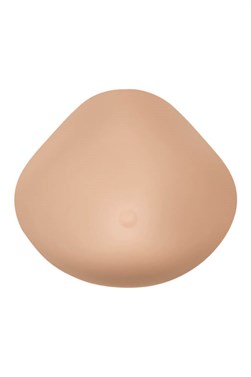
After reconstruction, if you still need a little help with balance and symmetry, Amoena is here.